AI-Designed Molecule Boosts Chemotherapy Response in Pancreatic Cancer
An AI-designed molecule made pancreatic cancer cells more vulnerable to chemotherapy in lab and preclinical tests.
A research group at the Italian Institute of Technology (IIT-Istituto Italiano di Tecnologia) has identified a candidate molecule that could improve current therapies against pancreatic cancer. The team designed the new molecule, called Apt1, using artificial intelligence tools and tested it in in vitro experiments, demonstrating its effectiveness in making tumour cells more vulnerable to chemotherapy drugs. When combined with drugs already in use, the molecule increases the effectiveness of anticancer therapies even at lower dosages than those normally given. The research study has been published in the scientific journal Nature Communications.
Gian Gaetano Tartaglia, head of the RNA Systems Biology laboratory, and Andrea Cavalli, head of the Computational and Chemical Biology laboratory, led the work alongside the Structural Biophysics Facility directed by Stefania Girotto.
In Italy, pancreatic cancer affects approximately 14,000 people every year and ranks among the most aggressive and difficult to treat, with a five-year survival rate of approximately 10% Therapeutic strategies remain limited to a few chemotherapy drugs and prompt surgical interventions. The scientific community actively searches for new solutions, studying drug responses across different pancreatic cancer subtypes.
The IIT research team focused on one specific drug, olaparib, to extend its effectiveness across different subtypes. Olaparib is an anticancer agent used in cases of breast or ovarian cancer in patients with BRCA mutations, and it is also prescribed for the treatment of pancreatic adenocarcinoma. It induces tumour cell death through a strategy known as synthetic lethality: a mechanism that exploits the genetic difference between healthy and diseased cells, targeting only the latter. Olaparib slows down DNA repair in tumour cells, forcing them to accumulate extensive DNA damage and thus inducing their destruction.
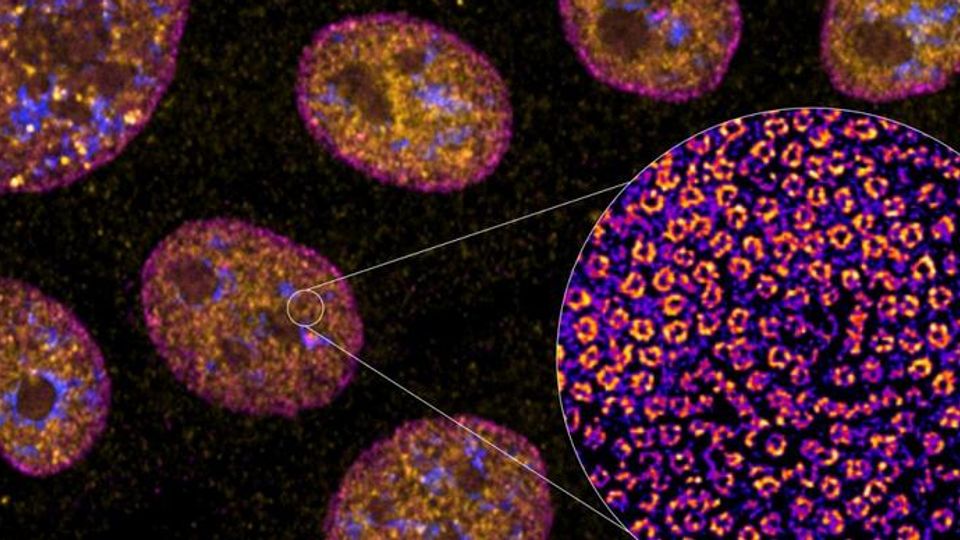
The IIT study focused on two proteins involved in DNA repair: RAD51, which corrects certain genetic errors, and BRCA2, which guides RAD51 to the damaged DNA site inside the cell nucleus. The research group devised a solution that hinders the interaction between the two proteins, thereby impairing the tumour cell's ability to replicate.
The identified solution is an aptamer, a small nucleic acid sequence RNA or DNA) designed to interact in a highly specific way with a target protein. The team designed it using an algorithm called catRAPID, developed by Tartaglia's group in previous works, which rapidly identifies aptamer sequences based on the proteins they must interact with.
Once they completed the computational work, the researchers obtained a list of aptamers and conducted initial laboratory experiments to identify the most promising one. A molecule called Apt1 emerged as the most relevant candidate, demonstrating strong binding to RAD51 and making it unreachable for BRCA2.
In subsequent phases, the research group tested Apt1 in pancreatic tumour cells. The experiments, designed and supervised by Giulia Milordini, IIT researcher and first author of the article, showed that Apt1 slows DNA repair, makes cancerous cells more vulnerable to chemotherapy drugs, and has limited effects on healthy cells. Finally, tests on preclinical models verified the strength of the combined action of olaparib and Apt1, demonstrating their greater capacity to attack cancerous tissues compared to when used individually.
The results show promise for moving toward clinical trials, with the goal of introducing a new therapeutic strategy where few treatment options currently exist.
Reference: Milordini G, Zacco E, Masi M, et al. Computationally-designed aptamers targeting RAD51-BRCA2 interaction impair homologous recombination and induce synthetic lethality. Nat Commun. 2025. doi: 10.1038/s41467-025-66694-9
This article has been republished from the following materials. Note: material may have been edited for length and content. For further information, please contact the cited source. Our press release publishing policy can be accessed here.