Lipid-Based Systems’ Potential To Transform CAR T Therapy for Solid Tumors
Dr. Kelemen discusses how lipid nanoparticles can improve CAR T delivery, tackle solid tumor barriers and offer a safer, scalable alternative to viral vectors.
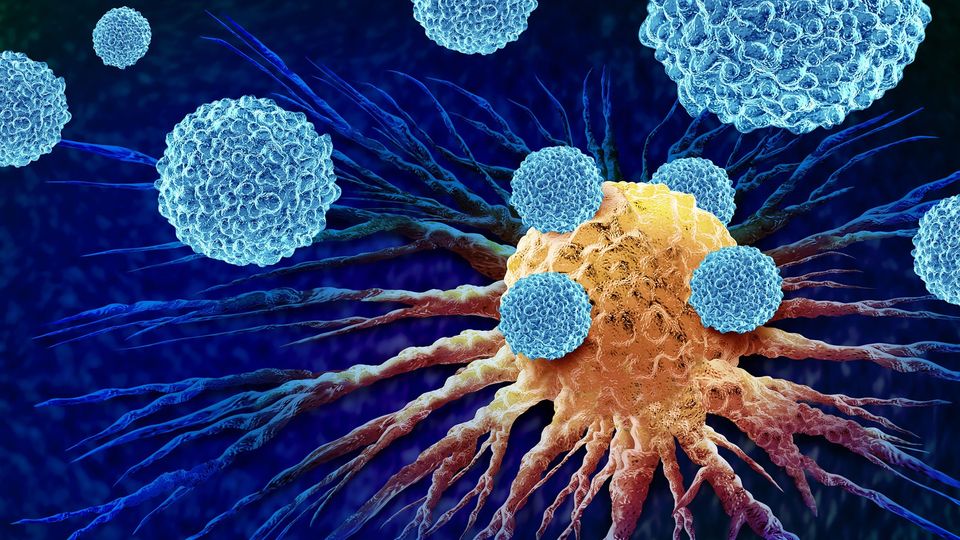
Although chimeric antigen receptor (CAR) T-cell therapies have shown encouraging results for treating hematological cancers such as leukemias and lymphomas, their success in solid tumors has so far been limited.
Solid tumors pose a range of physical, biological and logistical challenges that make them more difficult to target. Adding to these issues are the limitations of traditional viral vector delivery systems, which underscore the need for alternative delivery approaches.
Technology Networks recently spoke with Donald Kelemen, head of corporate business development and global business director, pharmaceutical at ABITEC, to explore solutions to these obstacles. In this interview,
What are the key challenges of viral vector-based delivery in the context of CAR T-cell therapy for solid tumors?
Developing viral vector–based CAR T therapies for solid tumors brings several unique challenges. One of the most significant is the tumor microenvironment, which brings physical and biological barriers. Abnormal vasculature can prevent CAR T cells from efficiently infiltrating the tumor, while immunosuppressive factors such as regulatory T cells and cytokines can suppress their activity once inside.
Also, with viral vectors, transduction efficiency can vary, making it difficult to achieve consistent therapeutic results and, in some patients, pre-existing immunity to viral components may compromise the effectiveness of the therapy altogether. Even when transduced successfully, CAR T cells may not efficiently migrate to or accumulate within solid tumors enough to drive a meaningful therapeutic response.
Lipid nanoparticles (LNPs) offer several advantages that make them well-suited to overcoming the challenges facing CAR T therapies in solid tumors. By encapsulating nucleic acid cargo, they protect it from degradation and potential immune attack within the tumor microenvironment. LNPs can also be engineered to co-deliver modulators such as checkpoint inhibitors, helping to counteract the microtumor suppression environment.
Another significant benefit is their reduced immunogenicity. LNPs are less likely to trigger immune responses than viral vectors, particularly when multiple doses are required, contributing to a more favorable overall safety profile.
There is no single technology that can address the specific delivery challenges in the cell and gene therapy field. Viral systems have played a critical role in the field to date, and they will continue to be used in the development of next-generation therapeutics. That being said, however, there is a growing interest in utilizing the functionality and capabilities of LNP systems as an alternative, with several factors driving this shift.
One of the most pressing issues in cell and gene therapy is patient safety. Integrating viral vectors, such as retroviruses or lentiviruses, carries the risk of insertional mutagenesis, which can disrupt host genes and potentially drive oncogenesis. They can also trigger strong immune responses, resulting in inflammation, clearance of transduced cells or other adverse events. In addition, uncontrolled or unintended gene integration can create unpredictable off-target effects in patients.
The manufacturing of viral vectors also creates a significant bottleneck. Viral vector production is technically complex, costly and time-intensive, particularly at GMP scale. Consistency between batches is difficult to achieve, which can complicate both product quality and regulatory approval. The high cost of manufacturing and scaling production, as well as patient administration, in turn restricts patient accessibility and can create challenges for reimbursement by healthcare systems.
There are also practical limitations in terms of design flexibility. Many viral systems have limited capacity to carry genetic material, which restricts the development of more complex therapies. Constructs that require multiplexed editing, larger CAR designs or additional immunomodulators often cannot be accommodated within the confines of viral vectors.
Regulatory considerations are further driving an interest in alternatives. The approval pathway for viral-based systems can be lengthy and demanding, whereas non-viral platforms may benefit from fewer barriers and a more streamlined review process. By reducing the regulatory burden, lipid-based systems could accelerate clinical development and support faster patient access.
In general, the move away from viral vectors is driven by safety, manufacturing, regulatory and practical limitations. Alternatives like LNPs, electroporation and synthetic carriers offer improved safety, scalability, flexibility and regulatory advantages, making them attractive for next-generation cell and gene therapies.
Again, there is no single approach or technology that can uniformly address the complex nature of construct design, payload integration, safety and regulatory challenges. The development of LNP therapeutics for cell and gene therapies is no different, and each program must address a set of technical challenges on a case-by-case basis.
One of the most immediate challenges is in vivo stability and biodistribution. LNPs are often rapidly cleared by the liver or spleen, reducing the amount that reaches the intended target cells. Depending on the lipid composition (e.g., PEG-lipids or certain ionizable classes), non-specific distribution may occur, raising the possibility of unintended gene editing in non-target tissues.
Reaching the right tissue in sufficient amounts also remains a critical barrier. LNPs must cross biological obstacles such as the blood–brain barrier or the solid tumor microenvironment, which can significantly limit delivery efficiency. Even once inside the cell, the genetic payload must remain stable and then be released at the right time and in the right way for editing to occur successfully.
Safety presents another critical challenge. High doses or certain lipid components may cause cytotoxicity or provoke adverse immune reactions, especially in repeat dosing regimens, which can narrow the therapeutic window.
Finally, quality control, such as ensuring batch-to-batch consistency in properties such as size, encapsulation efficiency, charge and stability, remains a significant challenge when meeting regulatory standards for safety and efficacy.
One of the clearest examples of LNP-based delivery success comes from the COVID-19 pandemic, where LNPs enabled the mRNA vaccine to be produced at a speed and scale that would have been impossible using another delivery vector. CAR T therapies can and will benefit from standardized, scalable LNP manufacturing processes, helping to make both personalized and “off-the-shelf” treatments more accessible and affordable.
Additionally, the regulatory success of LNP-based mRNA vaccines in the pandemic has helped pave the way for faster approval and acceptance of these technologies. As such, CAR T therapies using LNPs may benefit from the established regulatory frameworks, potentially reducing development time and costs, and leading to an increase in approvals.
Another lesson comes from the issue of pre-existing immunity. Unlike viral vectors such as AAV or adenovirus, LNPs are not subject to pre-existing immunity concerns, making repeat dosing feasible and expanding patient eligibility.
There are already real-world examples that demonstrate how lipid-based systems are transforming the cell and gene therapy landscape. Intellia Therapeutics, for instance, has advanced a Phase 3 program that uses its proprietary LNP technology to deliver CRISPR/Cas9 gene-editing components in vivo. By encapsulating a codon-optimized mRNA encoding Cas9 together with a human KLKB1-specific sgRNA within a multicomponent lipid system, the company has shown how these particles can efficiently carry complex gene-editing machinery to target cells.
Another landmark came from Alnylam Pharmaceuticals, which used LNPs to deliver siRNA for the treatment of hereditary transthyretin-mediated amyloidosis. This became the first FDA-approved RNAi therapeutic using LNPs, validating the use of lipid systems for gene silencing in clinical practice.
Today, momentum continues to build across the field, with around 160 companies worldwide now investing in the development of LNP and lipid-based systems for cell editing technologies, highlighting its growing role in shaping next-generation therapies.
Lipid-based delivery systems, especially LNPs, have already transformed the cell and gene therapy landscape by enabling safe, effective and scalable delivery of nucleic acids and gene editing tools. These successes provide a strong foundation for further innovation in CAR T and other advanced therapies. However, several important challenges remain before the full potential of LNPs in solid tumors can be realized.
One of the most pressing issues is extra-hepatic delivery. Achieving precise targeting of LNPs to T cells for ex vivo modification, or directly to tumor sites for in vivo CAR T generation, is technically difficult. Avoiding non-selective accumulation in the liver is critical, and researchers are now focusing on strategies such as targeting ligands and surface modifications to improve specificity for T cells or tumor cells.
The tumor microenvironment poses another significant obstacle. Its dense extracellular matrix, abnormal vasculature and strongly immunosuppressive milieu can all hinder LNP penetration and CAR T-cell function. To overcome this, researchers are developing novel strategies, including the use of ECM-degrading enzymes and microenvironment-modulating agents, to enhance CAR T resilience and LNP penetration.
Beyond the scientific and biological barriers, regulatory and intellectual property considerations add further complexity. From the earliest stages of design, developers must navigate evolving regulatory requirements, engage with authorities proactively and generate rigorous preclinical safety and efficacy data. At the same time, an in-depth understanding of the patent landscape and freedom-to-operate parameters is essential to ensure that new therapies can advance without legal or commercial barriers.
It is difficult to predict the future of LNP delivery technologies, given how quickly the field is advancing, but I believe that lipid nanoparticles will continue to gain prominence as a versatile platform for delivering genetic material, both in ex vivo and in vivo settings.
Emerging approaches will most likely include the use of polymeric and hybrid nanoparticles, as advances in synthetic polymers and hybrid systems will create new opportunities for safe, efficient and targeted delivery. At the same time, refinements in electroporation and microfluidic technologies are expected to provide rapid, scalable and less toxic methods of gene transfer for patients in need.



